At the beginning of our senior year in Nursing, in the summer of 69, we start with our 3 month rotation at Providence Lying in Hospital for obstetrical and gynecological nurses training.
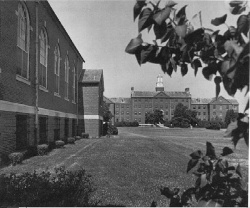
Providence Lying-In Hospital is a historic hospital building, located on 6 1/4 acres off Smith Street, in the Elmhurst section of Providence, situated at the end of a short access road, at 50 Maude Street, which leads directly into the grounds. The 1926 Collegiate Gothic style hospital is a four and a half story, red brick structure trimmed with Indiana limestone and capped by a slate, gable roof. Its most distinctive features are the six story central tower and a series of projecting bays combined with an overall fenestration pattern that provides a pleasing rhythm along the length of the building; allowing for a comfortable interior division of work space and patients’ accommodations while the numerous windows provide ample light and air circulation.
A course of limestone above the first floor level on all elevations is the single horizontal element of the original design and serves as a visual base for the bays and towers that extend upward. The central tower is turreted at each corner with a round cap drawn to a point. The point is extended upward by a wind vane whose decoration is a long, graceful stork in flight with a baby in a blanket suspended from its beak. The portion of the tower above the roof-line includes limestone reliefs of a winged cherub, an angel, and a mother and child. The tower has five bays at each floor. “Providence Lying-In Hospital is inscribed above the second story windows. The main entrance has limestone quoins on both sides and a flat Gothic arch. The door itself is a modern one of aluminum and glass. The window pattern of the main elevation is symmetrical above the second floor, bi-fold type that folds outward as the edges are drawn to the center. Each sash has ten panes. The Father’s waiting room has Gothic detailing and the main waiting area with wood paneling and a marble fireplace with a flat, Gothic arch.
The 1933 nurses’ residence is of similar materials, massive and style as the original hospital building with exception of the windows, which are six over six double hung sashes. The trim detail including the window and door quoins and course at the first story are cast stone rather than limestone. Dormers and pediment bays punctuate the slate roof-line in the manner of the original hospital building. There was an addition added in 1941, an auditorium and facilities for residents that faithfully continue the composition of the original construction.
The two buildings are joined by a two story hyphen, creating a broad “U” form surrounding a circular drive between the buildings. At the rear of the hospital is a two story, smooth faced concrete addition built in 1956. This infill structure joins two short wings extending from the old hospital building. The area surrounding the hospital is a landscape of mature deciduous trees, foundational plantings, and to the west is the large asphalt parking area bordered farther to the west by an undeveloped wooded parcel of land, with open spaces at the western perimeter of the property.
Incorporated in 1884 it is the first to provide on-going obstetrical services in RI and the first to offer specialized nurses’ training and on several occasions was recognized by leading national authorities on maternity care, who lauded it for its contribution to the development of the modern concept of a hospital devoted to healing and teaching- an attitude beyond the earlier notion of hospitals as institutions for the indigent. It pioneered the concept of caring for the emotional as well as the medical needs of its patients. Prior to its opening there was no place in the city where a woman, not living in her own home, could have in any measure proper care at confinement. Patients paid a stipulated price for the privileges afforded them by a well regulated hospital which was an attempt at removing the stigma around entering a hospital. The intent was to provide services for all classes of women, not only the poor, and it was supported by contributions.
In 1888 a training school for nurses was established offering generalized and specialized obstetrical training as well as post-graduate work and the first in RI to do so. In 1892 it established a department for the care of infants with specialized medical needs. The hospital is a manifestation of the social consciousness which was an outgrowth of the great industrial and economic expansion of the nineteenth century. It significant in the development of the modern concept of the hospital as an institution devoted to healing and caring for the sick and as a center for research and teaching.
Previously hospitals were built as “Rigs ward” which was copied extensively throughout the world and was a nightingale ward redesigned for more privacy. The ward plan named after Florence Nightingale provided efficient care of the patients by reducing the number of beds in a ward and locating the nurses’ station centrally within the ward. This structure was designed as a pavilion combining private rooms and a ward, greatly augmenting the proportion of private rooms. No ward was designed to hold more than six beds, this was indicative of the twentieth century trend towards greater privacy. Environment was seen as important including: the contour of the land, the surrounding country, the accessibility for friends to easily get to and from the city by roads and trolley, expressing cheerfulness, inspiring confidence, courage and dignity.
The above information is from The National Registry of Historic Places.
No matter where we are training our curiosity gets the better of us and we investigate our surrounds. We find a built in cabinet and open the large wooden doors and find ourselves looking at many shelves full of 5 gallon glass jars filled with fetuses and dead babies, many grotesque forms all in a row from the ceiling to the floor. We stand frozen in our places, not knowing what to make of the scene in front of us. We quickly close the doors and hurriedly leave the area, fearful of being caught, exposing a shocking secret, about the sorrowful side of birthing a child.
I experience the birth of many beautiful babies as they are welcomed to earth. I feel great sadness with the birth of babies with health issues. I am shocked and dismayed when a baby is born without any cranial bones thus seeing the formation of the brain while the doctor tells the parents the baby was born dead while he throws a drape over the delicate misshapen form, suffocating the new life without any compassion, and writes in the chart that the baby was a “monster”. Most of the babies in the state are born here.
We have our assigned patients who we follow through their pregnancy, labor, delivery and nursery. When they go into labor we are called in no matter what time of day or night it is. There are all varieties of birth from quick and easy to long and hard and many differences in between. The mothers can be screaming out in pain with each contraction, some even swearing at their husbands who are not there with them, while others breathe easily through the process. Our job is to hold their hands as they squeeze them tightly with the pain, instructing them on the proper breathing techniques, counting the minutes between contractions, and encouraging them to push when the time arrives, it’s an intense time.
It is an amazing experience, to watch the baby’s head crown, and be able to catch the small one in our hands. The umbilical cord is cut, the baby is held upside down by the feet and slapped on their tiny bottoms to get them to breathe, while they scream out in shock from being yanked out of the comfortable womb they have spent the last 9 months in. While the doctor is dealing with the placenta a pediatrician has taken the baby over to the side where a sterile field is set up on a table and the baby is suctioned with a bulb syringe to get amniotic fluid out of the mouth and receives a quick physical.
The baby is cleaned up, showed to the mother that it has all its limbs, and then quickly carried out to the viewing room. The baby is brought to the looking glass window for a close up look by the father and other family members present, in the long rectangular room you can see a few rows of clear see through bassinets on wheels, each containing a newborn, all swaddled in soft white cotton, some are quietly sleeping while others are crying to be held and cared for.
The mother is cleaned up then taken to her private room to rest briefly before we begin instructing on baby care. We bring the baby to the mother and teach breast or bottle feeding, caring for the umbilicus, bathing, encouraging bonding and caring for her baby on a regular scheduled time throughout the day/night. The room is large enough for the father and other family members to visit and spend time with the new mother and child.
We spend time in the nurseries where we care for the little ones with love and protection. There are a few of us together caring and playing with the babies when they are not with their mothers, picking them up when they are fussy or crying, it is so much fun and enjoyable interacting with these newborns. When in ICU it is a more intense situation and we are anxious and concerned over the health issues these tiny ones are experiencing, at times feelings of helplessness overwhelm me. I see the need for touch but they are in incubators and have minimal physical interaction because of the physical barriers so we talk to them and rock the machine. We rejoice when the infant is out of danger and is transferred to the nursery.
The issues coming to the forefront is the nurses caught stealing pain medications from the delivery room; there are no laws about controlled substances so record keeping is all based on what has been ordered and received. It creates a major scandal throughout the community. It is no surprise to me for since I have been in nursing school the students have been going to the pharmacy for menstrual cramps and have been given Percocet like they are candy, which seems to be over kill to me. Pain medications are all over the place and easily accessible, I am lucky that I am not tempted by them for it seems easy to become addicted. I am fearful of addiction to medications and any substance that is being sold out on the streets; I remain focused on my nursing studies and not wanting anything that will lead me off my path to my goal. I have received an excellent education in obstetrics and gynecological nursing and feel confident that I could do this work after graduation without too much fear or anxiety.